Allergic Rhinitis vs Sinusitis: How to Tell the Difference and Treat Each One
The key difference between allergic rhinitis and sinusitis is the cause: allergic rhinitis is an immune overreaction to harmless substances like pollen or dust mites, while sinusitis is inflammation or infection of the sinus cavities — usually triggered by a virus, bacteria, or fungus. Allergic rhinitis causes itchy nose and eyes, sneezing fits, and thin watery discharge. Sinusitis causes facial pressure, thick discolored mucus, and pain that worsens when bending forward. The two conditions frequently overlap — chronic allergic rhinitis is one of the leading risk factors for developing sinusitis — which is why treatment must address the right underlying cause.
Allergic Rhinitis vs Sinusitis: Quick Comparison
| Feature | Allergic Rhinitis | Sinusitis (Sinus Infection) |
|---|---|---|
| Cause | Immune reaction to allergens (pollen, dust, pet dander, mold) | Viral, bacterial, or fungal infection of sinus cavities |
| Nasal discharge | Thin, clear, watery | Thick, yellow, green, or cloudy |
| Itching | Yes — nose, eyes, throat, ears | Rarely |
| Sneezing | Frequent, often in fits | Occasional |
| Facial pain/pressure | Mild or absent | Significant — forehead, cheeks, between eyes |
| Fever | Never | Sometimes (especially bacterial) |
| Duration | As long as allergen exposure continues (weeks to months) | Acute: 7–10 days. Chronic: 12+ weeks |
| Pattern | Seasonal or year-round, tied to triggers | Follows a cold, or persistent after 10+ days |
| Sense of smell | Reduced during flares | Significantly reduced or absent |
| Contagious? | No | Viral sinusitis: yes. Bacterial: no |
What Is Allergic Rhinitis?
Allergic rhinitis occurs when your immune system identifies a harmless airborne substance — pollen, dust mites, mold spores, or pet dander — as a threat and releases histamine and other inflammatory chemicals in response. This triggers swelling of the nasal lining, excess mucus production, sneezing, and itching.
There are two types:
- Seasonal allergic rhinitis (hay fever): Triggered by outdoor allergens like tree pollen (spring), grass pollen (summer), and ragweed (autumn). Symptoms follow a predictable seasonal pattern. For management strategies, see our guide to stopping hay fever.
- Perennial allergic rhinitis: Triggered by year-round indoor allergens like dust mites, pet dander, cockroach droppings, and mold. Symptoms persist throughout the year but may worsen in winter when homes are sealed and heating systems circulate allergens.
What Are the Symptoms of Allergic Rhinitis?
- Itchy nose, eyes, throat, and sometimes ears
- Sneezing — often in rapid-fire fits of 5–10 sneezes
- Thin, clear, watery nasal discharge (rhinorrhea)
- Nasal congestion (stuffy nose)
- Watery, red, swollen eyes (allergic conjunctivitis)
- Dark circles under the eyes (“allergic shiners”)
- Postnasal drip with throat clearing
- Fatigue and brain fog from disrupted sleep and chronic inflammation
What Is Sinusitis?
Sinusitis (also called a sinus infection or rhinosinusitis) is inflammation of the mucous membranes lining the paranasal sinuses — the air-filled cavities behind your forehead, cheeks, nose bridge, and eyes. When the sinus openings (ostia) become blocked by swelling or thick mucus, fluid accumulates, pressure builds, and infection can develop.
According to the CDC, up to 98% of acute sinus infections are viral and resolve without antibiotics within 7–10 days.
What Are the Types of Sinusitis?
| Type | Duration | Common Cause |
|---|---|---|
| Acute sinusitis | Up to 4 weeks | Viral infection (cold or flu) |
| Subacute sinusitis | 4–12 weeks | Unresolved acute infection, bacterial |
| Chronic sinusitis | 12+ weeks | Persistent inflammation, nasal polyps, allergies |
| Recurrent sinusitis | 4+ episodes per year | Anatomical issues, immune deficiency, allergies |
What Are the Symptoms of Sinusitis?
- Thick, discolored nasal discharge (yellow, green, or cloudy)
- Facial pain and pressure — concentrated in the forehead, cheeks, or between the eyes
- Pain that worsens when bending forward or lying down
- Reduced or absent sense of smell and taste
- Nasal congestion and obstruction
- Post-nasal drip with thick, mucus-like throat coating
- Tooth pain (upper teeth, from maxillary sinus pressure)
- Bad breath (from bacterial activity in trapped mucus)
- Fever (more common with bacterial sinusitis)
- Fatigue and general malaise
How Do Allergic Rhinitis and Sinusitis Overlap?
These two conditions are deeply interconnected. Allergic rhinitis is one of the strongest risk factors for developing sinusitis, and they frequently coexist — a combination that ear-nose-throat specialists call allergic rhinosinusitis.
The chain of events typically works like this:
- Allergen exposure triggers immune-mediated swelling of the nasal lining
- Swollen tissue blocks the sinus openings (ostia), preventing normal mucus drainage
- Trapped mucus becomes a breeding ground for bacteria
- Bacterial infection develops — what started as allergic rhinitis becomes sinusitis
This is why treating the underlying allergy often prevents recurrent sinus infections. If you get 4+ sinus infections per year, undiagnosed allergies may be the root cause.
How Is Each Condition Diagnosed?
How Do Doctors Diagnose Allergic Rhinitis?
- Symptom history: Seasonal pattern, trigger identification, family history of allergies
- Skin prick testing: Small amounts of common allergens applied to the skin — a raised wheal within 15 minutes confirms sensitivity
- Blood test (specific IgE): Measures allergen-specific antibodies in your blood
- Nasal examination: Pale, boggy (swollen) nasal turbinates suggest allergic inflammation rather than infection
How Do Doctors Diagnose Sinusitis?
- Symptom duration and pattern: Symptoms lasting 10+ days without improvement, or “double sickening” (improving then worsening), suggest bacterial sinusitis
- Physical examination: Facial tenderness, purulent (pus-like) nasal discharge
- Nasal endoscopy: A thin flexible scope examines the sinus openings directly
- CT scan: Reserved for chronic sinusitis or suspected complications — shows fluid levels, mucosal thickening, and structural abnormalities
How Is Each Condition Treated?
Treatment for Allergic Rhinitis
| Treatment | How It Works | Speed | Best For |
|---|---|---|---|
| Nasal corticosteroid spray (Flonase, Nasacort) | Reduces inflammation at the source | 1–2 weeks for full effect | First-line treatment for moderate-severe symptoms |
| Antihistamine (cetirizine, loratadine) | Blocks histamine that causes sneezing and itching | 30–60 minutes | Sneezing, itching, runny nose |
| Saline nasal rinse | Flushes allergens from nasal passages | 5–10 minutes | Daily prevention + symptom relief |
| Allergen avoidance | Removes the trigger | Immediate | Foundation of all allergy management |
| Immunotherapy (allergy shots/drops) | Gradually desensitizes the immune system | Months to years | Long-term cure for persistent allergies |
For a detailed comparison of allergy sprays, see our guides to nose spray types for allergies and best allergy nasal sprays compared.
Treatment for Sinusitis
| Treatment | How It Works | When to Use |
|---|---|---|
| Saline nasal irrigation | Flushes mucus, bacteria, and debris from sinuses | All sinusitis types — first-line treatment |
| Steam inhalation | Thins mucus, opens swollen passages | Symptom relief during acute infection |
| Warm compress | Relieves facial pain and pressure | Pain management |
| OTC pain relievers (ibuprofen) | Reduces pain and inflammation | Facial pain, headache |
| Nasal corticosteroid spray | Reduces sinus inflammation | Acute and chronic sinusitis |
| Antibiotics | Kills bacterial infection | Only when bacterial sinusitis is confirmed (10+ days, double sickening, high fever) |
The CDC recommends saline nasal rinses, steam inhalation, and warm compresses as first-line sinus infection management, noting that most infections improve without antibiotics. For a complete home treatment protocol, see our guide to treating a sinus infection at home.
Can You Have Both Allergic Rhinitis and Sinusitis at the Same Time?
Yes — and it is common. Studies estimate that 40–80% of chronic sinusitis patients also have allergic rhinitis. When both conditions are present, treatment must address both:
- Treat the allergy (antihistamines, nasal steroids, allergen avoidance) to stop the inflammation that blocks sinus drainage
- Treat the sinusitis (saline irrigation, steam, antibiotics if bacterial) to clear the active infection
- Prevent recurrence with daily nasal steroid spray and regular saline nasal irrigation to keep sinus passages open
If you experience 4 or more sinus infections per year, ask your doctor about allergy testing — treating the underlying allergy often breaks the cycle of recurrent infections.
How Does This Compare to Allergies vs a Cold?
This is a related but different distinction. A cold is a viral upper respiratory infection with a defined timeline (7–10 days), while allergies persist as long as allergen exposure continues. For a detailed comparison of cold vs allergy symptoms, see our allergies vs cold guide.
Frequently Asked Questions
Can allergic rhinitis turn into a sinus infection?
Yes. Allergic rhinitis causes nasal swelling that can block the sinus drainage openings (ostia). When mucus is trapped behind these blocked openings, bacteria can multiply and cause a secondary sinus infection. This is why chronic allergy sufferers are significantly more likely to develop sinusitis. Treating the allergy — with nasal corticosteroid sprays, antihistamines, and saline nasal irrigation — helps prevent this cascade.
Why does my sinusitis keep coming back?
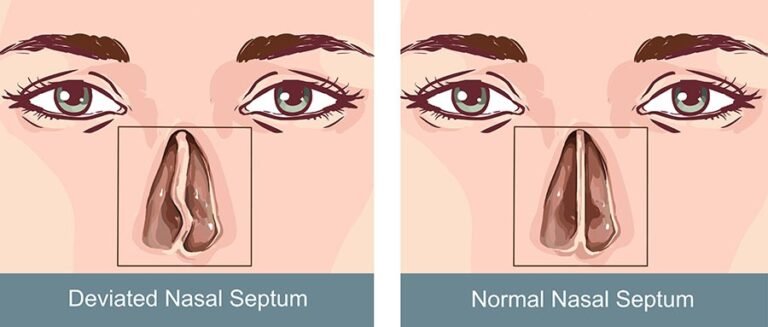
Recurrent sinusitis (4+ episodes per year) is often driven by an underlying condition that has not been addressed. The most common causes are undiagnosed allergies, nasal polyps, a deviated septum, immune deficiency, or acid reflux (GERD) that irritates the nasal passages. An ENT evaluation with nasal endoscopy and allergy testing can identify the root cause and guide targeted treatment.
Do I need antibiotics for a sinus infection?
Usually not. According to the CDC, up to 98% of acute sinus infections are viral and resolve within 7–10 days with supportive care (saline rinses, steam, hydration, rest). Antibiotics are only appropriate when symptoms last longer than 10 days without improvement, worsen after initially improving (“double sickening”), or include high fever with severe facial pain — signs that suggest bacterial rather than viral infection.
Is thick yellow mucus always a sign of sinusitis?
No. Yellow or green mucus indicates that your immune system is actively fighting an infection — the color comes from white blood cells (neutrophils) concentrated in the mucus. This happens with both viral colds and bacterial sinus infections. The color alone does not distinguish between the two. Duration and severity of symptoms are more reliable indicators: a cold with yellow mucus improving over 7–10 days is likely viral, while worsening symptoms beyond 10 days suggest possible bacterial sinusitis.
Can children have allergic rhinitis and sinusitis?
Yes. Children are particularly susceptible to both conditions. Allergic rhinitis affects up to 40% of children and is a major contributor to childhood sinusitis. Children’s sinus openings are smaller and more easily blocked by allergic swelling. Signs to watch for include persistent mouth breathing, snoring, dark circles under the eyes, and frequent throat clearing. A pediatrician or pediatric ENT can evaluate symptoms and recommend age-appropriate treatment.
Bottom Line
Allergic rhinitis and sinusitis share many symptoms but require different treatment approaches. The fastest way to tell them apart: itching and sneezing suggest allergies; facial pain and thick discolored mucus suggest sinusitis. In many people, the two conditions coexist and fuel each other — allergic inflammation blocks sinus drainage, creating the conditions for infection. Breaking this cycle requires treating both the allergy (nasal steroids, antihistamines, allergen avoidance) and the sinus symptoms (saline irrigation, steam, rest). If you experience recurrent sinus infections, allergy testing may reveal the underlying trigger and point toward a lasting solution.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Consult a healthcare provider for persistent nasal or sinus symptoms.