Post Nasal Drip Treatment: Causes, Remedies and When to See a Doctor
What Is Post Nasal Drip?
Post nasal drip occurs when excess mucus from the nasal passages and sinuses drains down the back of the throat rather than out through the nose. Your body produces one to two liters of mucus daily under normal conditions, and most of it is swallowed unconsciously. Post nasal drip becomes noticeable — and problematic — when the mucus is thicker than usual, produced in greater quantity, or your throat becomes irritated by the constant drainage.
The sensation is often described as a constant need to clear the throat, a feeling of something stuck in the back of the throat, or a persistent tickle that triggers coughing. Post nasal drip is one of the most common causes of chronic cough and sore throat in adults.
Common Causes
Allergies
Allergic rhinitis is one of the leading causes of post nasal drip. When allergens like pollen, dust mites, or pet dander trigger an immune response, the nasal membranes produce excess thin, watery mucus that drains backward. Seasonal patterns (worse in spring or fall) or year-round symptoms (dust mites, mold) help identify allergies as the cause.
Viral Infections (Colds and Flu)
Upper respiratory infections increase mucus production as the immune system fights the virus. The mucus often starts thin and clear, then becomes thick, yellow, or green as the infection progresses. Post nasal drip from a cold typically resolves within 7 to 10 days.
Sinus Infections (Sinusitis)
When the sinuses become infected, thick inflammatory mucus drains down the throat. Bacterial sinusitis produces particularly thick, discolored drainage that can persist for weeks if untreated. The drip is often accompanied by facial pressure and sinus pain.
Gastroesophageal Reflux (GERD and LPR)
Laryngopharyngeal reflux (LPR), sometimes called “silent reflux,” occurs when stomach acid reaches the throat and nasal passages. The acid irritates the mucous membranes, stimulating excess mucus production. Unlike typical GERD, LPR often causes throat clearing, hoarseness, and post nasal drip without obvious heartburn.
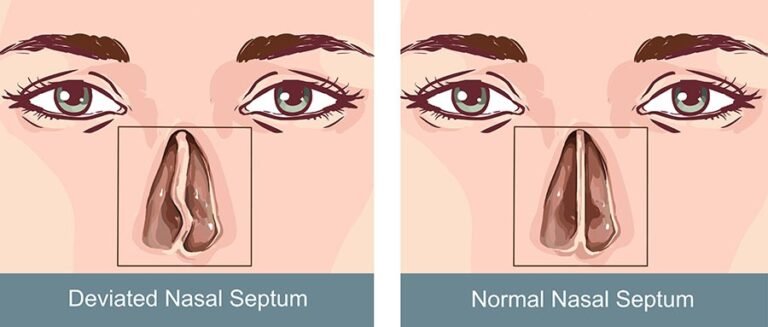
Deviated Septum or Nasal Polyps
Structural abnormalities can impair normal mucus drainage, redirecting flow to the throat instead of out through the nose. A deviated septum may cause one-sided post nasal drip, while nasal polyps can create bilateral drainage issues.
Dry Air and Environmental Irritants
Cold, dry air (especially from indoor heating systems) thickens nasal mucus, making it more likely to drip down the throat rather than flow out the nose. Smoke, strong perfumes, cleaning chemicals, and air pollution also irritate the nasal lining and increase mucus production.
Medications
Certain medications can cause or worsen post nasal drip. ACE inhibitors (blood pressure medications like lisinopril) are well known for causing a chronic dry cough and throat irritation. Birth control pills and some antidepressants can also thicken nasal secretions.
Treatment Options
Saline Nasal Irrigation
Flushing the nasal passages with saline is one of the most effective treatments for post nasal drip regardless of cause. The saline mechanically removes excess mucus, allergens, and irritants while thinning thick secretions so they drain more normally. Use a neti pot or squeeze bottle with distilled water two to three times daily.
Hypertonic saline (a slightly higher salt concentration) can be particularly helpful for thick post nasal drip because it draws fluid out of swollen tissues and helps thin stubborn mucus through osmosis.
Nasal Corticosteroid Sprays
Fluticasone (Flonase), triamcinolone (Nasacort), and budesonide (Rhinocort) reduce inflammation in the nasal passages, decreasing mucus production at the source. They are especially effective when allergies or chronic inflammation drive the post nasal drip. Use daily for at least one to two weeks to see full benefit.
Antihistamines
For allergy-related post nasal drip, second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra) reduce the allergic response driving excess mucus. First-generation antihistamines like diphenhydramine (Benadryl) have a stronger drying effect that can reduce post nasal drip from any cause, but cause drowsiness.
Azelastine (Astepro) nasal spray combines antihistamine action with direct nasal delivery for faster, more targeted relief.
Mucus-Thinning Agents
Guaifenesin (Mucinex) thins thick mucus, making it easier to clear from the throat and nasal passages. It is most helpful when post nasal drip involves thick, stubborn secretions rather than thin, watery drainage. Take with plenty of water for best effect.
Hydration and Warm Fluids
Staying well hydrated keeps mucus thin and flowing. Warm herbal teas — particularly peppermint, ginger, and honey-lemon blends — thin mucus, soothe the irritated throat, and provide anti-inflammatory benefits. Aim for at least eight glasses of water daily, more if you are taking a mucolytic like guaifenesin.
Steam Inhalation
Breathing warm, moist air loosens thick mucus and soothes the irritated throat lining. Inhale steam from a bowl of hot water (optionally with eucalyptus oil) for 10 to 15 minutes. A hot shower achieves a similar effect. Steam therapy is particularly useful before bed when post nasal drip often triggers coughing that disrupts sleep.
Elevate the Head While Sleeping
Lying flat allows mucus to pool in the throat, worsening the dripping sensation and triggering coughing. Sleeping with the head elevated 15 to 30 degrees — using an extra pillow or wedge pillow — promotes better drainage and reduces nighttime symptoms.
Treat Underlying GERD or LPR
If acid reflux is contributing to post nasal drip, treating the reflux often resolves the drip:
- Elevate the head of your bed six to eight inches (not just pillows — elevate the bed frame or use a wedge under the mattress).
- Avoid eating within three hours of bedtime.
- Reduce acidic, spicy, and fatty foods.
- Over-the-counter acid reducers like famotidine (Pepcid) or omeprazole (Prilosec) may be recommended by your doctor.
Humidity Control
Running a cool-mist humidifier maintains indoor humidity between 40 and 50 percent, preventing the nasal mucus from thickening due to dry air. This is especially important during winter when heating systems strip moisture from indoor air. Clean the humidifier daily to avoid mold growth.
Gargling for Throat Relief
Post nasal drip frequently irritates the throat, causing soreness and a persistent need to clear the throat. Gargling can provide symptomatic relief:
- Salt water gargle: Dissolve half a teaspoon of salt in eight ounces of warm water. Gargle for 30 seconds and spit. Repeat three to four times daily. The salt reduces throat swelling and helps thin mucus coating the throat.
- Honey gargle: Add a tablespoon of honey to warm water. Honey has mild antibacterial properties and coats the irritated throat.
When Is Post Nasal Drip Chronic?
Post nasal drip lasting more than two to three weeks is considered persistent and warrants investigation into the underlying cause. Chronic post nasal drip that lasts months or years is usually caused by:
- Undiagnosed or undertreated allergies
- Chronic sinusitis
- Silent acid reflux (LPR)
- Nasal polyps or structural issues
- Vasomotor rhinitis (non-allergic nasal inflammation triggered by weather, odors, or temperature changes)
When to See a Doctor
Seek medical evaluation if post nasal drip lasts more than two weeks without improvement, the drainage is thick, discolored (yellow or green), and accompanied by facial pain or fever (suggesting sinus infection), you notice blood-tinged mucus without an obvious cause, post nasal drip is accompanied by unexplained weight loss or difficulty swallowing, throat clearing and cough persist despite home treatment, or you suspect acid reflux may be contributing to your symptoms.
An ENT specialist can perform a nasal endoscopy to examine the sinuses and throat directly, order allergy testing, or evaluate for structural abnormalities that may require surgical correction.
Bottom Line
Post nasal drip responds best to treatment targeted at the underlying cause: antihistamines and nasal steroids for allergies, saline irrigation and time for infections, acid management for reflux, and humidity control for dry-air irritation. Saline nasal irrigation, adequate hydration, and warm fluids provide universal relief regardless of cause. For thick secretions, guaifenesin helps thin the mucus, while head elevation at night reduces the nighttime coughing and throat clearing that disrupt sleep. If symptoms persist beyond a few weeks, a doctor can identify the root cause and recommend targeted treatment.