Nasal Decongestant Guide: Types, Uses and Side Effects
What Is a Nasal Decongestant?
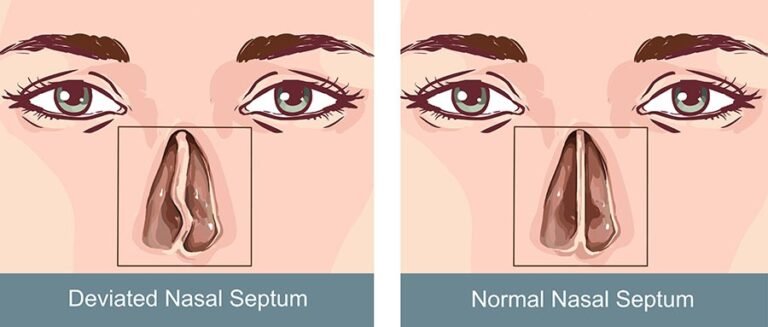
A nasal decongestant is a medication that shrinks swollen blood vessels and tissues in the nasal passages, opening the airway and making it easier to breathe. When you have a cold, allergies, or a sinus infection, the turbinates inside your nose become engorged with blood, narrowing the nasal passage. Decongestants work by constricting these blood vessels, which reduces the swelling and restores airflow.
Decongestants come in two main forms — oral (pills and liquids) and topical (nasal sprays). Each has distinct advantages, limitations, and risks that are important to understand before choosing the right option for your situation.
Types of Nasal Decongestants
Oral Decongestants
Pseudoephedrine (Sudafed)
Pseudoephedrine is the most effective oral decongestant available. It works systemically, meaning it constricts blood vessels throughout the body, including those in the nasal passages. Effects begin within 30 minutes and last 4 to 6 hours (immediate-release) or up to 12 hours (extended-release).
Availability: Available behind the pharmacy counter without a prescription. You must show identification and sign a logbook due to federal regulations (pseudoephedrine can be used to manufacture methamphetamine). Purchase limits apply.
Dosage: Adults typically take 30 to 60 mg every 4 to 6 hours (immediate-release) or 120 mg every 12 hours (extended-release). Do not exceed 240 mg in 24 hours.
Phenylephrine (Sudafed PE)
Phenylephrine is widely available on regular store shelves, but its effectiveness when taken orally has been questioned. In 2023, an FDA advisory panel unanimously concluded that oral phenylephrine is no more effective than placebo for nasal congestion. Despite this finding, it remains on the market. If you need reliable oral decongestant relief, pseudoephedrine is the evidence-backed choice.
Nasal Decongestant Sprays
Oxymetazoline (Afrin, Sinex)
Oxymetazoline is a topical decongestant that works directly on the nasal blood vessels. It provides rapid relief — typically within minutes — and lasts up to 12 hours per dose. It is the strongest OTC nasal decongestant spray available.
Dosage: Two to three sprays in each nostril every 10 to 12 hours. Do not exceed two doses in 24 hours.
Phenylephrine Nasal Spray (Neo-Synephrine)
Unlike the oral version, phenylephrine is effective when applied topically as a nasal spray. It works within minutes and lasts approximately 4 hours, making it shorter-acting than oxymetazoline.
Dosage: Two to three sprays in each nostril every 4 hours as needed.
Xylometazoline (Otrivin)
Available primarily outside the United States, xylometazoline is similar to oxymetazoline in mechanism and duration. It provides 8 to 10 hours of relief per dose.
How to Use Nasal Decongestant Sprays Correctly
Proper technique ensures the medication reaches the swollen tissue rather than dripping down the throat:
- Blow your nose gently to clear any excess mucus.
- Shake the spray bottle if directed on the label.
- Tilt your head slightly forward (not backward).
- Insert the nozzle into one nostril while closing the other nostril with a finger.
- Aim the spray toward the outer wall of the nose (away from the septum), not straight up.
- Squeeze the bottle while inhaling gently through the nose.
- Avoid sniffing hard, which pulls the medication past the nasal tissue and into the throat.
- Repeat on the other side.
- Avoid blowing your nose for several minutes after application.
The Rebound Congestion Problem
The most important warning about nasal decongestant sprays is the risk of rebound congestion, medically called rhinitis medicamentosa. When topical decongestants are used for more than three consecutive days, the nasal blood vessels begin to lose their ability to constrict on their own. When the medication wears off, the vessels dilate even more than before, creating worse congestion that drives repeated use.
This cycle can become self-perpetuating. Some people use decongestant sprays for weeks, months, or even years, unable to breathe without them. Breaking the cycle requires stopping the spray — which causes several days of intense congestion — or a supervised tapering approach using nasal corticosteroid sprays to manage withdrawal symptoms.
The three-day rule: Never use oxymetazoline, phenylephrine spray, or xylometazoline for more than three consecutive days. If congestion persists beyond that, switch to a different approach for sinus relief such as saline irrigation, nasal corticosteroid sprays, or oral decongestants.
Side Effects of Nasal Decongestants
Oral Decongestant Side Effects
- Increased blood pressure: Pseudoephedrine constricts blood vessels throughout the body, which can raise blood pressure. People with hypertension should avoid it or use it only under medical supervision.
- Increased heart rate: Palpitations and rapid heartbeat are possible, especially at higher doses.
- Insomnia: The stimulant effect can interfere with sleep. Take the last dose at least four to six hours before bedtime.
- Anxiety and restlessness: Some people experience jitteriness similar to excessive caffeine.
- Urinary retention: Men with enlarged prostate may have difficulty urinating.
- Dry mouth: Reduced salivary secretions are common.
Nasal Spray Side Effects
- Rebound congestion: The most significant risk with use beyond three days.
- Nasal burning or stinging: Temporary discomfort upon application.
- Dryness: The tissue-constricting effect can dry the nasal lining.
- Sneezing: Some people sneeze after application.
- Nosebleeds: Repeated use can irritate and dry the nasal mucosa, leading to minor bleeding.
Who Should Avoid Nasal Decongestants
Decongestants are not safe for everyone. Avoid or consult your doctor before using them if you have:
- High blood pressure (hypertension)
- Heart disease or irregular heartbeat
- Glaucoma (narrow-angle type)
- Hyperthyroidism
- Enlarged prostate (benign prostatic hyperplasia)
- Diabetes (pseudoephedrine can affect blood sugar)
- Pregnancy (decongestants may reduce placental blood flow)
Children under age 4 should not receive any OTC decongestant without pediatric medical guidance. For children ages 4 to 12, use pediatric formulations with appropriate dosing.
Nasal Decongestants vs Other Congestion Treatments
| Treatment | How It Works | Speed | Duration | Safe for Long-Term Use? |
|---|---|---|---|---|
| Pseudoephedrine (oral) | Constricts nasal blood vessels systemically | 30 minutes | 4 to 12 hours | Short courses only (7 to 10 days max) |
| Oxymetazoline (spray) | Constricts nasal blood vessels locally | Minutes | 10 to 12 hours | No — 3 days maximum |
| Fluticasone (nasal steroid) | Reduces inflammation | Days to build up | 24 hours (daily use) | Yes |
| Cetirizine (antihistamine) | Blocks histamine (allergy pathway) | 1 hour | 24 hours | Yes |
| Saline irrigation | Mechanically flushes passages | Minutes | 2 to 4 hours | Yes |
| Guaifenesin (mucolytic) | Thins mucus | 30 minutes | 4 to 12 hours | Yes |
Combination Products
Many cold and sinus medications combine decongestants with other active ingredients:
- Decongestant + antihistamine: Products like Claritin-D or Zyrtec-D combine pseudoephedrine with an antihistamine for allergy-related congestion with runny nose and sneezing.
- Decongestant + pain reliever: Advil Cold and Sinus pairs pseudoephedrine with ibuprofen for congestion with headache or facial pain.
- Decongestant + mucolytic: Mucinex D combines pseudoephedrine with guaifenesin for congestion with thick mucus.
When choosing a combination product, make sure you need all the active ingredients. Taking unnecessary medications increases side effect risk without added benefit. Also check that you are not doubling up on any ingredient by taking multiple products simultaneously.
Natural Alternatives to Decongestants
If you cannot take decongestants or prefer a drug-free approach, effective alternatives include:
- Saline nasal irrigation: Using a quality neti pot or squeeze bottle provides mechanical mucus clearance without any medication.
- Steam inhalation: Warm, moist air thins mucus and soothes swollen tissue.
- Menthol products: Vicks VapoRub and menthol lozenges create a sensation of improved breathing without actually changing blood vessel diameter.
- Warm herbal teas: Peppermint, eucalyptus, and ginger teas combine hydration with natural anti-inflammatory and decongestant compounds.
- Nasal strips: External strips like Breathe Right physically open the nasal valve for drug-free airflow improvement.
When to See a Doctor
Consult a healthcare provider if you need decongestants for more than seven to ten days, you suspect rebound congestion from prolonged spray use, congestion is accompanied by high fever and severe facial pain, you have a medical condition that makes decongestants risky, or over-the-counter treatments are not providing adequate relief. A doctor can evaluate the underlying cause and may prescribe targeted treatments such as prescription nasal sprays, antibiotics for bacterial infection, or refer you to an ENT specialist for structural evaluation.
Bottom Line
Nasal decongestants are powerful tools for short-term congestion relief, but they require careful use. Pseudoephedrine is the most effective oral option, while oxymetazoline spray works fastest for acute episodes. The critical rule is to limit spray decongestant use to three days to avoid rebound congestion. For ongoing or chronic nasal congestion, nasal corticosteroid sprays, saline irrigation, and antihistamines offer safer long-term alternatives. Always match the decongestant type to your specific cause of congestion and consult a pharmacist or doctor if you have underlying health conditions.